Progressive Resistance Training for Osteoporosis: How to Strengthen Bones Safely
Did you know that simply walking or lifting the same light weights every week won’t be enough to keep your bones strong? If you want to prevent osteoporosis, build bone density, and stay active for life, you need to progressively challenge your bones and muscles—and that’s where Progressive Resistance Exercise (PRE) comes in!

PRE is a scientifically backed strength training method that helps increase bone strength, reduce fracture risk, and improve stability—all crucial for women over 50 looking to maintain strong, healthy bones naturally.
What is Progressive Resistance Exercise (PRE)?
Progressive Resistance Exercise (PRE) is the gradual increase of resistance over time to stimulate muscle and bone growth. Instead of repeating the same exercises at the same intensity, PRE challenges your bones progressively, ensuring they continue to remodel and strengthen.
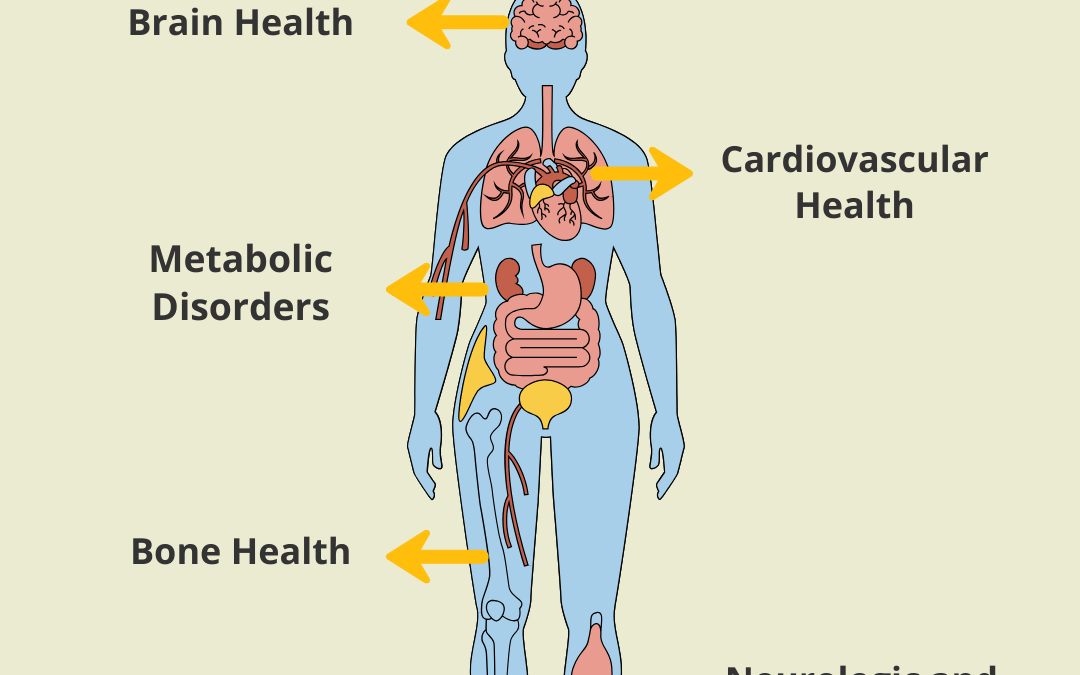
Key Benefits of PRE for Bone Health:
- Increases bone mineral density
- Reduces fracture risk
- Strengthens muscles that support bones
- Improves posture & balance (reducing falls)
- Prevents osteoporosis progression
Why Walking & Light Weights Aren’t Enough
Many women think that walking daily or lifting 3-5 lb dumbbells is enough to protect their bones. While these are great first steps, they don’t provide the progressive overload necessary for bone remodeling and strength gains.
-
- Walking is weight-bearing but lacks enough impact to stimulate significant bone growth.
- Lifting the same light weights without progression doesn’t challenge bones enough to grow stronger.
- Osteoporosis-prone areas (hips, spine, and wrists) need targeted strength training to build resilience.
If you want to truly strengthen your bones, you MUST progressively increase resistance over time!
How to Safely Progress Exercise
1. Start with Proper Form & Light Resistance
Women with osteoporosis should begin with bodyweight exercises or light resistance bands before moving on to weights. Proper form and alignment are essential to prevent stress on the spine and joints.
Beginner Example: Bodyweight squats, wall push-ups, seated leg lifts.
2. Gradually Increase Load and Resistance
Once comfortable, increase resistance slightly by adding light dumbbells or resistance bands. Small progressions, such as adding 1-2 lbs of weight every few weeks, allow bones and muscles to adapt safely.
Progression Example: Move from bodyweight squats to goblet squats with a 5-lb weight.
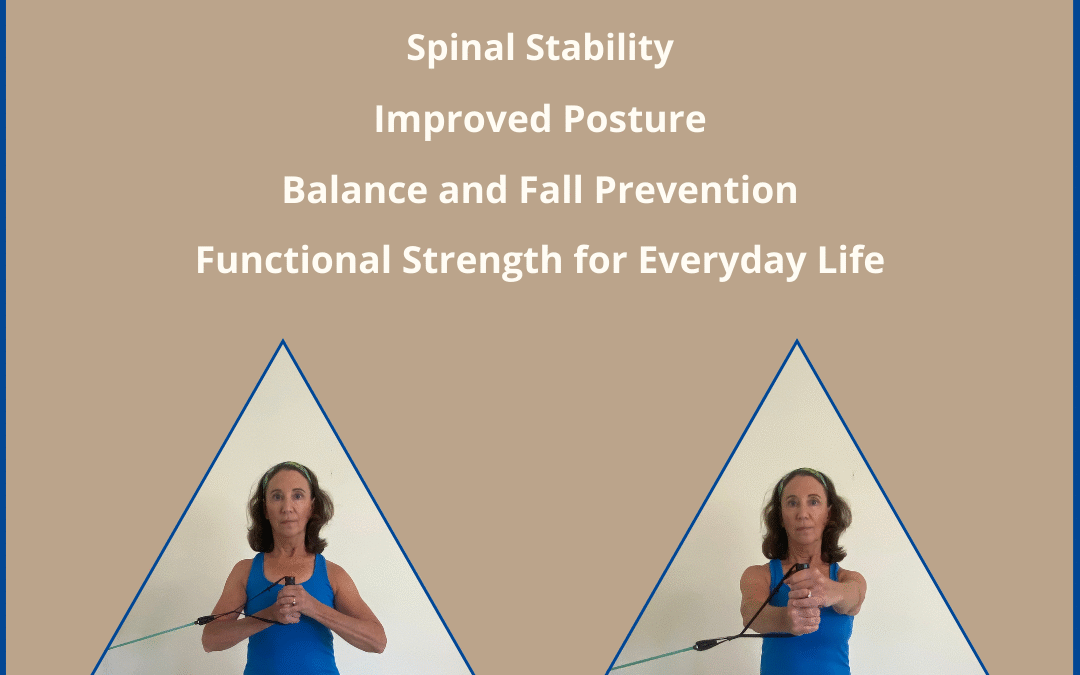
3. Focus on Key Bone-Building Areas
The most common fracture sites in osteoporosis are the spine, hips, and wrists. Exercises should specifically target these areas:
-
- Hips & Lower Spine: Squats, lunges, step-ups, leg presses.
- Upper Spine & Arms: Push-ups, bicep curls, triceps extensions, rowing exercises.
- Core & Stability: Planks, bridges, Pallof Press (check out my Pallof Press Blog for more on my favorite core strengthening exercise.)
4. Maintain a Safe Progression Pace
Avoid sudden increases in weight or impact. Progressing too quickly can lead to injury. Instead:
-
- Increase weight by 5-10% every 2-4 weeks.
- Perform 8-12 repetitions per set to maximize bone stimulation.
- Listen to your body—pain is a sign to modify, not push through.
Who Should Avoid Heavy-Weight Training?
While progressive loading is beneficial, women with severe osteoporosis or previous fractures should work with a qualified specialist to:
-
- Modify exercises that involve spinal flexion (e.g., crunches, forward bending).
- Ensure proper posture and alignment to protect the spine and joints.
The Takeaway: Strong Bones Need Progressive Challenge
Building stronger bones isn’t about doing more of the same exercises—it’s about progression. Gradually increasing resistance through Progressive Resistance Exercise (PRE) is one of the best ways to:
-
- Stimulate bone remodeling
- Prevent fractures and falls
- Enhance posture, balance, and mobility
Whether you’re just starting out or looking to advance your training, a properly designed progressive strength program can help you maintain strong, healthy bones for life.
Ready to Start a Bone-Strengthening Exercise Plan?
If you’re unsure how to safely build strength without increasing fracture risk, I can help. Let’s create a personalized plan that aligns with your bone health needs and fitness level.
Schedule a consultation today!
Scientific Research on Strength Training & Bone Health
Multiple studies confirm the effectiveness of resistance training for bone strength:
A study published in the Journal of Bone and Mineral Research found that high-intensity resistance training significantly increased bone density in postmenopausal women. (Weidauer et al., 2015)
Another study in the Osteoporosis International Journal highlighted that progressive resistance training reduces fracture risk and improves muscle mass in older women. (Kelley et al., 2018)
Research from the National Osteoporosis Foundation suggests that weight-bearing & resistance training are essential for osteoporosis prevention and management. (NOF, 2023)